Introduction
Bringing the early segment of genesis back to life was the totally dedicated and undivided obsession of Michelangelo, the greatest artist, painter and sculptor the world has ever known. During the peak of the Italian Renaissance period Michelangelo gave the world the life like sculptors of 'Moses', 'David', 'Madonna Della Pieta' and the 'Bond Slave'.
Imagine this greatest sculptor was living with us today and we happen to provide him the best available materials, tools, equipment and technologies of our era. If we were also successful in persuading the maestro to duplicate the hands of a particular human being, can this great artisan recreate the elevated, intricate patterns of his subjects fingerprint? POSSIBLY NOT! The reason being the formation of these aberrant ridges that we see on the skin of our fingertips is the most sophisticated individualistic intricate creation of the human body[1]. What appear to be the haphazard patterns of broken lines are in reality the pre coded chromosomal characteristics of our individuality.
Fingertips, the characteristic elevated ridge patterns on the fingertips of humans, are unique to each individual. The fingers and toes, the palms of the hands and soles of the feet, are covered with a system of ridges, which form certain patterns[1]. The term Dermatoglyphics is applied to both the configurations of the ridges, and also to the study of fingerprints. Beside the medico-legal importance of the ridge patterns of fingerprints, characteristic Dermatoglyphic abnormalities frequently accompany many chromosomal aberrations[1].
Early studies on papillary patterns of human fingers were reviewed by Bonnevie; it was concluded as early as 1892 by Galton that fingerprint patterns are inheritable. Based on the studies of inherited patterns and pattern sequences in ten fingers a genetic theory was developed by Slatis et al[1].
Aggressive periodontitis (AgP) comprises a group of rare, often severe, rapidly progressive forms of periodontitis often characterized by an early age of clinical manifestation and a distinctive tendency for cases to aggregate in families. An interesting thing is some individuals with poor oral hygiene suffer little periodontal destruction, while others with little plaque have advanced periodontal destruction[2]. What makes those individuals developing the disease different from others? Two hypotheses have been proposed to account for this variation:
• Certain plaque bacteria have a greater potential for tissue destruction than others and when they are present disease will occur.
• Host factors determine the tissue response to plaque[2].
The following key characteristics of AgP prompted us to leverage Dermatoglyphics as a bio-indicator to study its occurrence.
• Familial Linkage: AgP has been characterized by an early age of clinical manifestation and distinctive tendency to aggregate in families. AgP differs from the chronic form primarily by rapid rate of disease progression seen in an otherwise healthy individual, an absence of large accumulation of plaque and calculus[3] and a family history of aggressive disease suggestive of genetic trait. Given that Dermato glyphics is largely determined by Genotype, we expect a strong linkage.
• Escaping Early detection:An absence of large accumulation of plaque and calculus, the gingivae shows very few signs of clinical inflammation, which makes it harder to arrive at early symptoms. Study of this form can act as an early warning.
• Aggressiveness and severityThe aggressive nature of the disease which is seen in the later part of the teenage with rapid attachment loss and bone destruction can be avoided when a patient is identified with such a possibility.
For the first time, we are attempting to use Dermatoglyphic as a bio-indicator to establish patient’s susceptibility to develop AgP through this study.
We discuss various work that has been performed both in the area of Dermatoglyphics as a bio-indicator to uncover some of the hard genetic related diseases and disorders and also works to find the cause of AgP in section 3 of this paper under brief literature survey, materials and methods used for our experiment in section 4 and key approach to data collection in section 5 and the results, discussion and inference in section 6. We finally present our conclusion in section 7.
Brief Literature Survey
Dermatoglyphics has been a useful tool in understanding basic question in biology, medicine and genetics and at times serves as a tool to predict occurrences and risks for biomedical events. Extensive investigations in to chromosomal disorders like Down syndrome, Turner’s syndrome etc. and their Dermatoglyphics manifestations have been conducted[4]. Significant investigations have also been carried for the Dermatoglyphics indicators of breast cancer, celiac disease, rubella, tuberculosis[5], schizophrenia, glaucoma. It has been a boon to study occurrences of a lot of hereditary diseases and disorders. Variation from the healthy normal type of fingerprint occurs in many human disorder and diseased condition[6].
Dermatoglyphics has been used to unveil oral diseases like dental caries, oral cancer, bruxism, malocclusion, anomalies of teeth, cleft lip, cleft palate, period ntal disease, dental fluorosis and also in unveiling truth with forensic odontology[7], [8], [9], [10], [11], [12], [13], [14], [15], [16], [17], [18], [19], [20].
Presentation of AgP early in the life of an individual implies that etiologic agents have been able to cause clinically detectable levels of disease over a relatively short time. Inspite of this, AgP escapes early detection because
1. The gingivae shows very few signs of clinical inflammation and
2. Supra and sub-gingival plaque and /or calculus deposits are usually absent.
Inspite of its rare occurrence AgP has been the focus of many investigations aimed at understanding its etiology and pathogenesis because of the severity and aggressiveness with which it presents in a patient. Hence, it is of utmost importance to identify the patients who are at high risk of manifesting AgP[2].
Given the severity and tendency to progress, early detection of AgP should be primary concern of both practitioners and public health officers. The whole, including young children and young adults, should receive a periodontal screening as part of their routine dental examination.
Aggressive forms of periodontitis are currently considered to be multifactorial diseases developing as a result of complex interactions between microbiologic agents, specific host genes, immunologic and the environment/ behavioural risk factors which decide the the onset, course and severity of this disease[3],[21]. Several family studies have indicated that the prevalence of AgP is disproportionately high among certain families[3].
The aim of the present study is determine the occurrence of specific Dermatoglyphics pattern variation in AgP patients with special reference to fingertip pattern, to correlate the findings in patients that of the control cases (normal persons) and to establish the prevalence of a specific fingertip pattern that can be type casted to be susceptible to AgP.
Materials and Methods:
Subjects for the study included 30 diagnosed and treated patients of AgP from the Department of Periodontics, Government Dental College, Bangalore and from other private clinics over a period of five years. Subjects also included, 30 control cases not suffering from AgP were taken for comparison.
Approach to Data Collection
The present study was conducted to evaluate fingertip patterns of patients aged between 20 to 35 yr., diagnosed with and treated for AgP (study group) and normal individuals (control group) to observe a degree of divergence in the two groups and prevalence of any specific pattern in the study group. The subjects for the present study included 30 patients in the study group and 30 healthy normal individuals in the control group. We have limited this study to the extent of discussing only the major patterns. Finger tip pattern were recorded and analyzed according to the standard guidelines for classification of patterns.
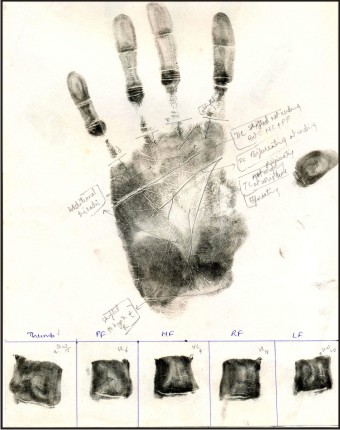
Patient’s consent was taken before recording the prints. Patient’s hands were cleaned and dried. Thin layer of Black Kajal material was applied to the fingers and palm using the eyetex Kajal stick. Imprints of fine fingertips were recorded in specified boxes by rolling the finger from one side. The entire palm print was recorded in the middle of the A4 sheet. Prints were dried and studied using a magnifying lens to identify the finger and palm patterns. After taking the finger prints of all the finger and palm, ink was removed using oil, soap and water.
Various patterns of fingers & palm were analyzed according to the standard guidelines for classification of patterns[22]. The following are the basic pattern types that occur in finger tips. These types of pattern depend upon the number of triradii (a triradius is a point formed by the meeting of three different ridge fields).
1. Arch which has no or only central triradius.
a. Simple arch (SA) - Simplest configuration with no triradius as shown below.
b. Tented arch (TA) - has a central triradius as shown below.
2. Loop which has one triradius – Designated as ulnar (UL) or radial (RL) depending upon the margin of the hand to which it opens as shown below.
3. Whorl which has two or more triradii.
a. Single loop whorl (SLW) as shown in figures below.
b. Double loop whorl (DLW) as shown below.
Arches and radial loops have the lowest overall frequency. When present they occur most often on digit 2(PF). Ulnar loops occur more frequently than any other pattern type. The most frequent combination of patterns is ten ulnar loops. Pattern frequencies vary somewhat with side and sex, females having slightly more arches and fewer whorls than males. There are also racial differences: Orientals have a higher frequency of whorls than Europeans and Americans[22].
Results, Discussion and Inference:
Part A1:Study Group: Right fingertip pattern prevalence.
Part A2:Study Group: Left fingertip pattern prevalence.
Part B1:Control Group; Right fingertip pattern prevalence.
Part B2:Control Group; Left fingertip pattern prevalence.
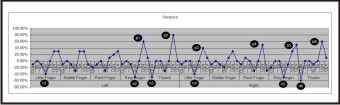
The results themselves clearly indicate that there is a huge variance between the study and control group. We took this initial result to transform them into a variance report to study if there are any specific patterns in conjunction with finger which we can observe. We present that data to show the spikes of variance that can be seen are interestingly spread on both sides of the x-axis as depicted in Figure 1. The positive variances which are numbered p1 to p6 indicate the absence of a pattern which is found in normal cases. These are:
• ULN in Left Ring Finger as shown by p1
• ULN in Left Thumb as shown by p2
• ULN in Right Little finger as shown by p3
• ULN in Right point finger as shown by p4
• ULV in Right Ring finger as shown by p5 and finally
• ULN in Right Thumb as shown by p6
 | Variance Seen Among Patient Cases As Against Narmal Cases
 |
 | Palm And Finger Tip Dermatoglyphic Pattern In An Aggressive Periodontitis Patientshowing Double Loop Whorl Pattern On Thumb Tip
 |
The negative variances which are numbered n1 to n6 indicate the presence of a pattern which is not found in normal cases. These are:
• SLW in Left little Finger as shown by n1
• SLW in Left Ring Finger as shown by n2
• DLW in Left Thumb as shown by n3
• SLW in Right Little Finger as shown by n4
• SLW in Right Ring finger as shown by n5 and finally
• DLW in Right Thumb as shown by n6
It is very evident from the variance report that there is a strong coherence of negative and positive variances for four fingers. They are constituted by the following pattern combinations:
• Left Ring Finger: Presence of SLW (n2) and Absence of ULN (p1)
• Left Thumb: Presence of DLW (n3) and Absence of ULN (p2)
• Right Little Finger: Presence of SLW (n4) and Absence of ULN (p3)
• Right Ring Finger: Presence of SLW (n5) and Absence of ULV (p5)
• Right Thumb: Presence of DLW (n6) and Absence of ULN (p6)
We can further filter this by the intensity of variance into three main pattern combinations:
• Left Ring Finger: Presence of SLW (n2) and Absence of ULN (p1)
• Left Thumb: Presence of DLW (n3) and Absence of ULN (p2)
• Right Thumb: Presence of DLW (n6) and Absence of ULN (p6)
There are very few studies relating dermatoglyphic patterns to periodontitis. There are only two articles relating dermatoglyphics to periodontitis in English literature. Our observation of dermatoglyphic patterns in aggressive periodontitis patients is similar to the results of a study done by M. Atasu, B. Kuru, E. Firatli, H. Meriç.According to their study in a periodontal condition co-related to dermatoglyphics a decreased frequencies of twinned and transversal ulnar loops on all fingers of the patients with Juvenile Periodontitis (aggressive periodontitis) was found[23], which coincides with our observation of absence of ULN in our group of patients. M. Atasu et. Al also observed that there is decreased frequency of double loops on all fingers and an increased frequency of radial loops on the right second digits of the patients with Rapidly progressing periodontitis, and where as the patients of Acute Periodontitis showed increase in frequencies of concentric whorls and transversal ulnar loops[23]. In our study there is increased frequency (60%) of DLW on left and right thumb of study group and presence of SLW (60%) on left ring fingers of study group.
Conclusion:
It was our hypothesis that Dermatoglyphics can be a strong bio-indicator to find susceptibility to AgP due to the familial nature of its occurrence. Our data confirms this hypothesis. Through this experiment, we could isolate four main patterns that stood out in our variance analysis which happen to be absence of ULN and ULV and presence of DLW and SLW. We finally conclude that there are three specific pattern combinations which can be useful in studying the susceptibility of AgP.
This study done on a larger population with similar approach can be used as a screening test to find person’s susceptibility to AgP and thus ensure that the patients can be more cautious to prevent manifestations of AgP. We also believe that further correlation done amongst the isolated patterns may fine tune the ability to find person’s susceptibility to AgP.
Abbreviations:
ULN - Ulnar Loop Normal
Th - Thumb
ULV - Ulnar Loop Variations
PF - Point Finger
SLW - Single Loop Whorl
MF - Middle Finger
DLW - Double Loop Whorl
RF - Ring Finger
RL - Radial Loop
LF - Little Finger
TA - Tented Arch
SA - Simple Arch
AgP - Aggressive Periodontitis
References
1. Lin C. H, Liu. J. H, Osternurg. J. W and Nicol. J. D, Fingerprints comparison. I:Similarity of Fingerprints, Journal of Forensic Sciences, JFSCA, Vol. 27, No. 2, April 1982, pp. 290-304.
2. Maurizio S Tonetti, Andrea Mombelli . Aggressive Periodontitis, Book of Clinical Periodontology and Implant dentistry , chapter 19, Page 428, 2009.
3. Meyer J, Lallam-Laroye C, Dridi M. Aggressive periodontitis – what exactly is it? J Clin Periodontol 2004; 31: 586–587.
4. Marilyn Preus and F Clarke Fraser, Dermatoglyphics and Syndrome (Dec 1972), American J Dis Child, Vol 124.
5. Geetha Viswanathan, et al, Analysis of Fingertip Dermatoglyphics of tuberculosis patients at Bangalore, Journal of ecobiology, 14(3), 205-210, 2002.
6. Shaumann B, Alter M. et al, Dermatoglyphics in medical disorders. New York: Springer-Verlag, 1976.
7. Mathew L, Hegde AM, Rai K Dermatoglyphic peculiarities in children with oral clefts. J Indian Soc Pedod Prev Dent. 2005 Oct-Dec;23(4):179-82.
8. Ahmed RH,Aref MI,Hassan RM,Mohammed NR Dermatoglyphic Study on Patients with Dental Caries Who Wearing Dental Fillings and its Correlation to Apoptosis that Induced by Using Dental Fillings Nature and Science 2010;8(10):54-57.
9. Tyagi R,Khuller N, Sharma A, Khatri A Genetic Basis of Dental Disorders: A Review J Oral Health Comm Dent Oct 2008;2(3):55-6.
10. Sharma A, Somani R. Dermatoglyphic interpretation of dental caries and in correlation to salivary bacteria interactions: an in vivo study.J Indian Soc Pedod Prev Dent. 2009 Jan-Mar;27(1):17-21.
11. Atasu M Dermatoglyphic findings in dental caries: a preliminary report. J Clin Pediatr Dent. 1998 Winter;22(2):147-9.
12. Singh N,Sharma A,Goel D,Singhal A,Khera T,Sharma A Is dermatoglyphics a reliable criteria for quantifying oral and systemic diseases- A review Indian Journal of Forensic Medicine &Toxicology 2010 4(2):41-4.
13. Sharma A ,Palvi,Kapoor D Dermatoglyphics, Dentistry and Diagnosis-A Review Baba Farid University Dental Journal 2010 1(2):45-8.
14. Tikare S, Rajesh G, Prasad KW, Thippeswamy V, Javali SB Dermatoglyphics--a marker for malocclusion? Int Dent J. 2010 Aug;60(4):300-4.
15. Reddy S, Prabhakar AR, Reddy VV A dermatoglyphic predictive and comparative study of Class I, Class II, div. 1, div.2 and Class III malocclusions. J Indian Soc Pedod Prev Dent. 1997 Mar;15(1):13-9. 17.Kargül B, Alcan T, Kabalay U, Atasu M. Hypohidrotic ectodermal dysplasia: dental, clinical, genetic and dermatoglyphic findings of three cases.J Clin Pediatr Dent. 2001 Fall;26(1):5-12.
16. Atasu M, Biren S.Ellis-van Creveld syndrome: dental, clinical, genetic and dermatoglyphic findings of a case.J Clin Pediatr Dent. 2000 Winter;24(2):141-5.
17. Atasu M, Cimilli H.Fusion of the permanent maxillary right incisor to a supernumerary tooth in association with a gemination of permanent maxillary left central incisor: a dental, genetic and dermatoglyphic study.J Clin Pediatr Dent. 2000 Summer;24(4):329-33.
18. Yilmaz S, Atasu M, Kuru B A genetic and dermatoglyphic study on periodontitis.J Marmara Univ Dent Fac. 1993 Sep;1(4):297-306.
19. Atasu M, Ozbayrak S, Eryilmaz A.Generalized microdontia and associated anomalies: a clinical, genetic, radiologic and dermatoglyphic study.J Clin Pediatr Dent. 1996 Winter;20 (2):161-72.
20. Polat MH, Azak A, Evlioglu G, Malkondu OK, Atasu M The relation of bruxism and dermatoglyphics.J Clin Pediatr Dent. 2000 Spring;24(3):191-4.
21. T. Roshna and K. Nandakumar. Generalised aggressive periodontitis and its treatment options: case reports and literature review; Case reports in Medicine, volume 2012, article ID 535321.
22. James. R. Miller, et al, Dermatoglyphics in pediatric practice, Journal of paediatrics,1966, Vol 69, issue 2. Pages 302-312.
23. M. Atasu, B. Kuru, E. Firatli, H. Meriç. Dermatoglyphic findings in periodontal diseases. International Journal of Anthropology; JANUARY – JUNE 2005, Volume 20, Issue 1-2, pg. 63-75.
|